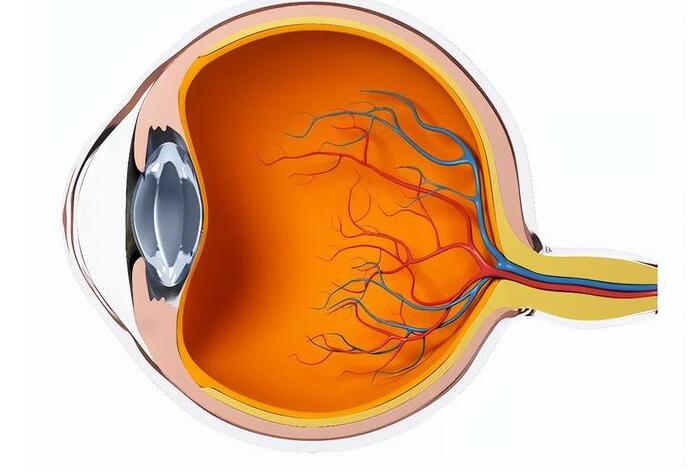
Diabetic retinopathy, a common and potentially vision-threatening complication of diabetes, poses a significant threat to the eyesight of millions worldwide. When our bodies struggle to manage blood sugar effectively, the persistent hyperglycemia can wreak havoc on the tiny blood vessels in the retina, leading to their weakening and propensity to leak or rupture. Over time, this can result in bleeding, scarring, and severe vision impairment, with blindness as the most feared outcome.
The Stages of Diabetic Retinopathy
Non-proliferative diabetic retinopathy (NPDR) marks the early stages, wherein retinal microaneurysms and exudates form due to vascular leakage. As these changes progress, they can lead to further complications.
Proliferative diabetic retinopathy (PDR), a more advanced stage, sees the growth of new, fragile blood vessels on the retina. These vessels are prone to bleeding, which can cause the retina to detach, leading to severe visual impairment or blindness.
Risk Factors
- Poor Glycemic Control: Chronically high blood glucose is the primary risk factor.
- Duration of Diabetes: The longer an individual has diabetes, the higher the risk.
- Hypertension: Elevated blood pressure exacerbates retinal vascular damage.
- High Cholesterol: Elevated cholesterol levels can also intensify retinal injury.
Symptoms and Diagnosis
Initially asymptomatic, signs may include blurred vision, dark spots, visual distortion, night vision loss, and color perception difficulties. Regular eye examinations are critical for early detection.
Treatment Modalities
Treatment varies with the severity and stage of diabetic retinopathy, and should be personalized:
- Glycemic Control: Vital for prevention and slowing the progression of diabetic retinopathy.
- Blood Pressure and Lipid Management: To reduce the risk of worsening retinopathy, employing medication and lifestyle adjustments.
- Pharmacotherapy: Includes hypoglycemic agents, antiplatelets, vasoprotective agents, and local treatments like anti-VEGF injections for macular edema relief.
- Laser Therapy: Photocoagulation techniques target non-proliferative changes or halt new vessel growth in PDR.
- Surgery: Vitrectomy for severe cases or complications, with cryotherapy as a less common alternative or adjunct to laser treatment.
- Regular Monitoring: Comprehensive eye examinations, including dilated fundoscopy and fluorescein angiography, are essential for early detection and monitoring.
Prevention Strategies
- Monitoring Blood Sugar: Keeping levels within the recommended range can prevent or delay retinopathy.
- Controlling Blood Pressure and Cholesterol: Essential for minimizing vascular damage.
- Regular Eye Examinations: Annual comprehensive eye exams are crucial for early detection.
- Quitting Smoking: Smoking exacerbates vascular damage, increasing complication risks.
- Balanced Diet: A diet rich in vegetables, whole grains, lean proteins, and healthy fats helps manage diabetes and its complications.
- Regular Exercise: Helps control blood sugar and may reduce the risk of retinopathy.
- Medication Adherence: Ensure timely medication intake as prescribed by your doctor.
- Moderate Alcohol Consumption: Excessive drinking can affect glycemic control.
- Managing Emotional and Stress Responses: Stress management is key to maintaining stable blood sugar levels.
- Awareness of Family History: If hereditary factors are present, discuss more frequent monitoring and preventive measures with your doctor.
While these strategies do not guarantee immunity from diabetic retinopathy, they significantly lower its progression risk. Regular communication with healthcare providers for personalized preventive plans is essential.
In conclusion, safeguarding our “windows to the soul” against diabetic retinopathy requires a combination of stringent glycemic control, proactive screening, lifestyle adaptations, and responsive treatment strategies. By staying vigilant and informed, we can effectively protect our vision and continue to enjoy the clarity of the world around us.